Device-Measured Sleep Duration Age 9–11 Years Among Urban Korean Children
Article information
Abstract
Objective
Sleep duration measurement methods are expensive and inconvenient. Smart bands or wearable activity trackers have offered objective and continuous tracking over several nights in real-world conditions. This study explored device-measured sleep duration in Korean children aged 9–11 years old.
Methods
This cross-sectional study, conducted between October 2022 and March 2023, enrolled 72 participants aged 9–11 years and equipped with smart bands (Xiaomi Mi Smart Band 6) for several nights lasting more than 5 days, including weekends. Sleep duration and sleep onset time were obtained using the smart bands.
Results
Seventy-one children (43 girls, 28 boys), with a mean age of 9.92±0.73 were included. Sleep durations on weekdays and weekends did not show a significant difference (8.55±0.66 h vs. 8.76±0.72 h). However, significant difference was observed in sleep onset time between weekdays and weekends (p<0.001). The sleep duration on weekdays and weekends declined with age. The sleep duration on weekdays and weekends was similar in each age group; however, the sleep onset time significantly differed for all age groups (p<0.05).
Conclusion
This study suggests insufficient sleep duration among the children in this study. And digital device may be an effective and fast way to evaluate children without a sleep laboratory, and suggest the need for further research to understand their implications and develop more accurate measurement methods for understanding children’s sleep.
INTRODUCTION
Sleep is essential for children’s growth and development, as well as their overall well-being. Children require adequate sleep for various aspects of their development. Sufficient sleep plays a vital role in helping children retain and consolidate the information they learn during the day, which, in turn, supports their cognitive development and academic performance [1,2]. Moreover, lack of sleep in early childhood has been consistently associated with an increased risk of obesity and adiposity [3-5].
When it comes to measuring sleep duration, objective methods such as polysomnography or actigraphy can provide more precise and detailed information about sleep duration and other sleep parameters. However, these methods have limitations, including high costs and discomfort. Contrastingly, self-reported sleep duration is commonly used in sleep screening and epidemiological studies because of its ease of use. However, recall bias or inaccuracies in reporting when relying solely on self-reports is a major concern. Furthermore, self-reported sleep duration may not capture brief awakenings or differences in sleep stages, thereby limiting the precision of collected data [6]. Despite these limitations, a systemic review found that sleep duration has predominantly been assessed subjectively [7]. Particularly in children, self-reported sleep duration has been used as the predominant method.
Wearable activity trackers, also known as smart bands, have recently gained popularity in monitoring various health aspects, including sleep duration. These devices offer the advantage of objective and continuous monitoring of sleep duration over multiple nights. However, comparative data assessing the accuracy and reliability of wearable devices is limited relative to research or clinical measurements.
This study aimed to assess the sleep duration of Korean children aged 9–11 years over multiple nights and to provide insights into the measurement of sleep duration using digital devices.
METHODS
Study participants
This cross-sectional study was conducted in Seoul and the metropolitan area near Seoul (Gyeonggi-do) with elementary students in grades three to five between October 2022 and March 2023. The exclusion criteria were neurological diseases, including attention-deficit hyperactivity disease, epilepsy, and autism. Trained field staff explained the smart band equipment and administered a basic questionnaire to the students and parents.
Students’ sex, age, and date of birth were obtained using a basic questionnaire. Weight (kg) and height (cm) were measured by authorized clinical staff, and body mass index (BMI) was calculated.
Seventy-two children aged 9–11 were enrolled and equipped with a smart band (Mi Smart Band 6; Xiaomi Communications Co., Ltd., Anhui, China) over multiple nights lasting more than 5 days, including weekends. The sleep duration and sleep onset time were directly extracted from the smart bands. Previous studies have shown that this device can reliably measure sleep duration of sleep [8,9].
Informed consent was explained to all students and their parents, and signed by both the students themselves and their parents or guardians voluntarily before participating in the study. This study was approved by the Korea University Ansan Hospital Institutional Review Board (IRB no. 2022AS0214).
Statistical analysis
Statistical analyses were performed using SPSS Statistics (version 25.0; IBM Corp., Armonk, NY, USA). Descriptive analyses were performed using means and standard deviations and frequencies or percentages. Time is presented as military time and converted to hours for statistical analysis. The Wilcoxon singedrank test for paired data were used to compare values.
RESULTS
This study finally enrolled 71 participants (28 males and 43 females). One participant was excluded because of insufficient equipment. The mean age was 9.92±0.73 years, with a mean weight was 46.09±9.96 kg and mean BMI was 20.38±3.65 kg/m2. Days on equipment for smart band are 14.10±7.33, with 10.40± 7.20 weekdays and 3.70±2.43 days on weekends (Table 1). Table 1 shows the anthropometric data of the participants according to sex.
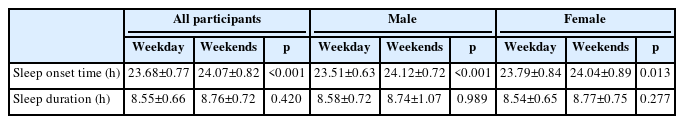
Sleep duration on weekdays was 8.55±0.66 h, and that on weekends was 8.76±0.72 h, which did not show a significant difference (p=0.420). However, significant difference was found in sleep onset time between weekdays (23.68±0.77 h) and weekends (24.07± 0.82 h) (p<0.001) (Table 2).
Sleep duration decreased with age on both weekdays and weekends (Figure 1). The weekday sleep duration was 8.78±0.48 h for 9-year-olds, 8.61±0.78 h for 10-year-olds, and 8.41±0.63 h for 11-year-olds. The weekend sleep duration was 8.96±0.81 h for 9-yearolds, 8.76±1.01 h for 10-year-olds, and 8.64±0.82 h for 11-year-olds. No significant difference in sleep duration was observed between weekdays and weekends in each age group. However, sleep onset time between weekends and weekdays significantly differed for all age groups (p<0.05)
Regarding sleep duration by sex, there was no difference in sleep duration on weekdays and weekends, as well as sleep onset time on weekdays and weekends, for both boys and girls (Table 2). However, for sleep onset time, both boys and girls showed a difference between weekdays and weekends, with significantly later bedtimes on weekends (p<0.05).
DISCUSSION
The accurate assessment of sleep duration may be useful as an indicator of children’s health and well-being. In this study, we collected data on sleep duration and sleep onset time from a digital device (a smart band) for multiple nights. For participants aged 9–11 years, the device-measured sleep duration was less than 9 h on weekdays and weekends. To the best of our knowledge, this study is the first to assess sleep duration and sleep onset time in Korean children using wearable devices over multiple nights. The study results suggest that the participants had shorter sleep durations based on the National Sleep Foundation’s sleep duration recommendations; 9–11 h of sleep per day is recommended for school-aged children [10]. The sleep onset time was approximately midnight, which showed difference between weekdays and weekends.
Sleep duration has been found to be influenced by environmental and genetic factors, showing variations across different populations and cultures [11,12]. Sleep studies found that sleep duration of children decreases progressively with advancing age, with delayed bedtimes and wakeup times [13,14]. Furthermore, across the globe, sleep duration has become shorter and late bedtime compared to previous decades [13-16]. This results for short sleep duration and late sleep onset time were similar to those of previous sleep studies in Korean children. Late bedtime may be influenced by external factors such as social demands, academic workload, or electronic device use. Children may underreport sleep duration due to time spent on activities like studying, using screens, or engaging in social interactions [17]. A study that examined sleep patterns and school performance in Korean adolescents found that nighttime sleep duration decreased significantly with increasing age [18]. During the weekday night, 5–6th graders slept for 7.95±1.05 h, 7–9th graders for 7.57±1.05 h, and 10–12th graders for 5.78±1.13 h. However, the total amounts of combined daytime and nighttime sleep during weekdays were somewhat greater, with 8.15±1.12 h for 5–6th graders, 8.17±1.20 h for 7–9th graders, and 6.87±1.40 h for 10–12th graders. A study analyzing age-related changes in sleep/wake patterns among Korean teenagers found that as children transitioned from childhood to adolescence, shifts occurred in sleep/wake patterns, resulting in later sleep onset and sleep deprivation among teenagers in Western societies [19].
Recent sleep patterns of Korean children have shown longer sleep duration on weekends than on weekdays and a late sleep onset time. A study in 2010, 5–6th grade in Korea, sleep duration and bedtime of weekdays are 7.95±1.05 and 23.13±0.58, and sleep duration and bedtime of weekends were 9.23±2.12 and 23.26± 1.07 h, respectively [20]. Kim et al. [21] reported that the sleep duration of 5th grader Korean children in 2012 was 8.3±-0.7 h on weekdays and 8.8±0.8 hon weekends. In a 2015 study [22], the self-reported sleep durations of healthy children aged 11 years were as follows: weekday sleep duration, 8.58±0.78 h; weekend sleep duration, 9.45±1.07 h; weekday bedtime, 22.84±0.72 h; weekend bedtime, 23.23±0.86 h.
The sleep duration of Korean children also exhibits differences compared to that of children in Western countries. Other pediatric sleep studies in Western and Asian countries have shown that sleep duration is longer and went to bed earlier than those of Korean children. A study with children in China conducted in 2010 showed that sleep duration was 9:10±0:56 h on weekdays and 10:04±0:55 h [23]. In a sleep study conducted with urban China children, the average sleep duration of 5–8th grade students was 9.43±0.70 h [24]. In Canada, sleep duration and bedtime of 10–11 years old children have been reported as 9 h 35 min and 21 h 29 min, respectively [25].
Digital devices for sleep tracking, such as wearable sensors and smartphone-based software applications, are powerful technologies that have become increasingly small in size and user-friendly [26]. Smart bands for sleep tracking use various mechanisms to monitor sleep patterns and quality. These devices often employ built-in sensors and algorithms to track sleep parameters, including sleep duration and quality. Smart bands monitor the time at which you are inactive and determine when you fall asleep at night and wake up in the morning. It incorporates heart rate sensors to estimate sleep stages and analyze sleep cycles [27]. Heart rate variability during sleep can provide insights into sleep quality and identify specific sleep stages like rapid eye movement (REM) and deep sleep.
Our study has several limitations. First, due to the small number of study participants, it may not be representative. However, this is an objective result compared to a self-reported study in which the sleep duration of subjects was measured for multiple nights over five days. Second, although commercially available sleep-tracking devices are becoming increasingly popular, there have been concerns about their validity against polysomnography [28,29]. Several studies have shown the validity of these trackers compared to gold standard sleep measurements [30-33]. De Zambottie et al. [31] reported that the sleep-wake monitor using Fitbit devices was fairly accurate relative to polysomnography. In addition, Xie et al. [32] reported good measurement accuracies and stabilities of wearable devices for sleep duration. Tal et al. [33] reported a high degree of correlation between software records and polysomnography records for total sleep time.
Despite these limitations, it is worth noting that while smart bands can provide valuable information about sleep duration, they may not be as accurate as clinical sleep measurement methods, such as polysomnography. Factors such as device placement, movement artifacts, and individual variability can introduce some degree of measurement error [34]. Nevertheless, smart bands offer a convenient and accessible way to monitor sleep duration and gain insight into sleep patterns for general use and self-assessment as low-cost technological tools under real-world conditions. Therefore, when used in conjunction with other objective measures and clinical assessments, smart band data can contribute to a comprehensive understanding of children’s sleep patterns and their impact on health outcomes.
This study suggests insufficient sleep duration among the children in this study. And digital device may be an effective and fast way to evaluate children without a sleep laboratory, and suggest the need for further research to understand their implications and develop more accurate measurement methods for understanding children’s sleep.
Notes
Funding Statement
This study was funded by the Ministry of Health & Welfare, Republic of Korea (Grant number: HS22C0036). Also, this study was financially supported by Hansung University for Byoung Gook Loh.
The authors have no potential conflicts of interest to disclose.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualizations: Won Hee Seo. Data curations: Byoung Gook Loh. Formal analysis: Byoung Gook Loh. Methodology: Eungu Kang, Young-Jun Rhie. Writing—original draft: Won Hee Seo. Writing—review and editing: Eungu Kang, Young-Jun Rhie.