Early Onset Depression Has Different Characteristics from Middle-Aged Depression in Terms of Circadian Rhythm
Article information
Abstract
Objective
The aim of this study was to identify the unique biological and circadian rhythmic characteristics of patients with early-onset depression compared to patients with middle-age-onset depression.
Methods
A total of 240 subjects were recruited in the study and divided into three groups: healthy young individuals, patients with early-onset depression, and middle-aged patients with unipolar depression. Patients then filled out questionnaires related to biological rhythm disturbances, mood symptoms, diurnal preference, and seasonality.
Results
Patients with early-onset depression had significantly different clinical features in terms of mood disorders, diurnal preference, and biological rhythm disturbances compared to middle-aged patients with unipolar depression.
Conclusion
Results of this study suggest that early-onset depression is different from middle-age-onset unipolar depression but similar to bipolar disorder.
INTRODUCTION
Despite bipolar disorder being a major debilitating mental illness, approximately 60% of patients with bipolar disorder are initially diagnosed with major depressive disorder (MDD) [1,2]. Some studies revealed that many people diagnosed with depression have bipolar disorder, most of whom are not diagnosed as being bipolar [3-5]. In particular, a study demonstrated that 27% of patients initially diagnosed with depressive disorder developed hypomanic episodes while 19% of patients developed full bipolar manic episodes [6]. Misdiagnosing a patient with bipolar disorder experiencing a depressive episode as having unipolar depression may cause several negative consequences, including inappropriate pharmacological prescriptions [7].
Several demographic and clinical characteristics are common between bipolar disorder and unipolar depression, including an early onset of illness (early 20s) and seasonality [8]. The Mood Disorder Questionnaire (MDQ) is a widely used screening instrument for bipolar disorder in patients with depression [9]. Emerging evidences suggest that circadian rhythm dysregulations could be a unique pathogenetic mechanism in bipolar disorder [10-17]. In particular, evidences suggest that acute mood episodes in bipolar disorder are related to circadian misalignment [14].
Biological rhythm is a concept that comprehends cyclic variations of both physiological and behavioral functions [18]. The Biological Rhythms Interview of Assessment in Neuropsychiatry (BRIAN) is a validated instrument that assesses the four main areas of circadian rhythm disturbance in bipolar disorder, namely sleep, social rhythm, activity, and eating pattern [19]. Previous studies reported that biological rhythmic disturbances in subjects with bipolar disorder can be considered as a trait marker of the disease [19,20] and also a trait for distinguishing bipolar disorder from MDD [21-23].
The purpose of this study was to identify and better understand the unique characteristics of early-onset depression by comparing the self-reported biological rhythms of patients with early-onset depression with those of patients with middle-age-onset MDD.
METHODS
Participants
A total of 240 participants were recruited in the study and divided into three groups: early-onset MDD (eMDD), late-onset MDD (lMDD), and healthy control (HC) groups. The eMDD group comprised 165 individuals with early-onset depression as part of the Mood Disorder Cohort Research Consortium study (ClinicalTrials.gov: NCT03088657) [24]. These patients were either under 35 years of age and had completed less than 2 years of treatment or under 25 years of age and had been diagnosed with MDD using the Mini-International Neuropsychiatric Interview [25]. The lMDD group comprised 35 patients diagnosed with MDD according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [26] and either aged over 35 years with over 2 years of treatment or aged over 45 years. These patients were recruited from the psychiatry outpatient clinic of the Korea University Hospital. The HC group comprised 40 individuals recruited from the general population of young adults [27]. All study participants were informed in detail about the purpose and procedures of the study prior to signing an informed consent form. The study protocol was approved by the Institutional Review Board of the Korea University Hospital (IRB No: 2018AN0446) and was conducted in accordance with the Declaration of Helsinki.
Assessments
All 240 participants were evaluated using clinical scales, including the Korean version of BRIAN, Korean version of MDQ [28], Korean version of Morningness-Eveningness Questionnaire (MEQ) [29], Korean Self-Rating Version of the Quick Inventory of Depressive Symptomatology (QIDS) [30], and Korean translation of the Seasonal Pattern Assessment Questionnaire [31]. Furthermore, sociodemographic characteristics of participants at the first visit were recorded. MEQ is a questionnaire for evaluating diurnal preference (also referred to as chronotype or morningnesseveningness trait). Patients with a higher MEQ score were considered to have increased morningness, reflecting earlier peaks in diurnal activity and energy and an advanced sleep-wake cycle. We investigated seasonal variations with the global seasonality score (GSS), a sum score of the degree (0–4) of seasonal variation of six items: sleep length, social activity, mood, energy level, body weight, and appetite, ranging from 0 to 24. A higher GSS indicates higher seasonal variations, which implies a higher possibility of having seasonal affective disorder, also known as winter depression [31].
Statistical Analysis
Statistical analyses were carried out with SPSS, version 22.0, for Windows (IBM Corp., Armonk, NY, USA). Comparison of sociodemographic and clinical variables between three groups was performed using the chi-square test and analysis of variance (ANOVA), followed by a pairwise comparison using Scheffe’s method. In case of unequal variances, Welch’s test and Dunnett T3 test were performed in three-group comparisons, followed by a pairwise comparison with ANOVA and Scheffe’s method, respectively. We performed Pearson’s correlation test for the correlation analysis of the age and total BRIAN score in the lMDD group. Results of the analysis were considered at a nominal significance of p<0.05.
RESULTS
Demographic and Clinical Characteristics of Participants
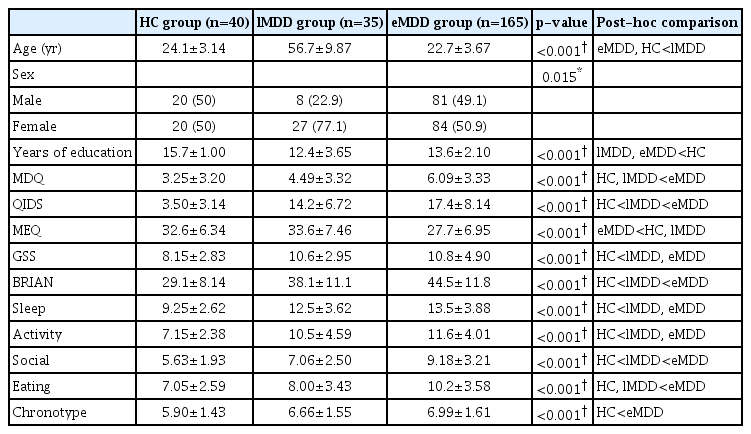
Among the total 240 participants, 40, 35, and 165 were in the HC, lMDD, and eMDD groups, respectively. Table 1 shows the demographic and clinical characteristics of the sample. Patients in the lMDD group were older than those in the HC or eMDD group based on the inclusion criteria. Females accounted for a larger proportion of the lMDD group compared to the HC or eMDD group. Participants in the HC group had more years of education compared to those of other groups.
Comparison of clinical and biological rhythmic characteristics between patients with eMDD, patients with lMDD, and HC based on questionnaire answers
All clinical variables (MDQ, QIDS, MEQ, and GSS) investigated in this study showed significant differences in the three-group comparison. In the subgroup analysis, the eMDD group showed significant differences in MDQ, QIDS, and MEQ results compared to the lMDD group. Only GSS showed no significant difference between the eMDD and lMDD groups. The HC and lMDD groups showed no significant difference in the MDQ or MEQ score. The eMDD group showed a significant difference in MDQ, QIDS, and MEQ results and GSS compared to the HC group.
Differences of Biological Rhythms between eMDD and lMDD Groups
The total BRIAN score and all five subscales showed significant differences among the three groups. In the subgroup analysis, the eMDD group had significantly higher total BRIAN score and scores of two subscales (social activity, eating pattern) than the lMDD group. Significant differences were found in the total score and scores of all subscales between the eMDD and HC groups. In eating and chrono subscales, the lMDD group scored higher than the HC group, but without statistical significance.
We checked the correlation of the total BRIAN score and age in the lMDD group since the age range in the lMDD group was relatively wide and evenly distributed. Age in the lMDD group ranged from 40 to 77 years, and the correlation coefficient r with the total BRIAN score was -0.073 (p=0.661). This result has not been displayed in the table.
DISCUSSION
According to the current diagnostic criteria, individuals with early-onset depression without apparent manic or hypomanic symptoms may be diagnosed with unipolar depression, also called MDD. However, we expected that a significant proportion of patients in the eMDD group could undergo bipolar conversion. In contrast, individuals in the lMDD group are supposed to be confirmed with unipolar depression in relation to their age and treatment duration.
Results from the analysis implied that the eMDD group had unique characteristics compared to the lMDD and HC groups. In particular, the eMDD group had more disturbances in biological rhythms than the lMDD group, particularly in social activity and eating patterns. Influences of age on biological rhythmic disturbances is still not well-known. Nevertheless, in our lMDD group, the total BRIAN score did not correlate with age. In addition, the mean total BRIAN score in the middle-aged control group of a large multi-center study [32] conducted at three locations (Spain, Brazil, and Canada) was similar to that in the young-age control group in our study.
Moreover, the mean total BRIAN score of bipolar II disorder in previous studies conducted in Korea [27,33] was close to that of the eMDD group in our study. However, there is no cut-off BRIAN score distinguishing bipolar disorder from MDD, and most individuals in the eMDD group demonstrated a significant amount of biological rhythmic disturbances similar to those with bipolar II disorder.
The MDQ score was also higher in the eMDD group than in the lMDD group. The best cut-off MDQ score was 6 or 7, distinguishing between bipolar disorder and MDD [34]. This also implies the heterogeneous nature of the eMDD group composed of pure unipolar depression and bipolar disorder.
Interestingly, the MEQ score of the eMDD group was significantly lower than both lMDD and HC groups, which implies increased eveningness in the eMDD group. One possible explanation is that individuals in the eMDD group are susceptible to circadian phase delay, thus having more chances of circadian misalignment leading to disturbances in biological rhythms and even depressive episodes. Next, we could suppose that susceptibility to circadian phase delay following disturbances in biological rhythms, seasonality, an early age of onset, and frequently recurrent depressive episodes are common characteristics shared by patients with early-onset depression and patients with bipolar II disorder but not those with typical middle-age-onset unipolar depression.
The main limitation of our study was the relatively small number of individuals in the HC and lMDD groups. Moreover, participants in the HC group were young and age distribution was narrow (mean age: 24.1±3.14 years). Nevertheless, the relationship between BRIAN and aging was not well established, but in our sample, age was not related to the BRIAN score.
In this study, we demonstrated distinguishable biological rhythmic features of patients with early-onset depression. Compared to typical patients with middle-age-onset unipolar depression, those with early-onset depression have similar aspects to patients with bipolar II disorder. In particular, the eMDD group scored higher on MDQ and had higher disturbances in biological rhythmicity in the BRIAN questionnaire compared to the lMDD group.
Furthermore, the unique characteristics of the eMDD group can be explained by the circadian rhythm hypothesis of bipolar disorder in that they are similar to the characteristics of bipolar disorder. Our results suggest alternative ways to understand early-onset depression, which can lead to appropriate diagnosis and treatment.
Acknowledgements
This study was supported by the Korea Health 21 R&D Project funded by the National Research Foundation of Korea (2017M3A9F1031220 and 2019R1A2C2084158).
Notes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Heon-Jeong Lee. Formal analysis: HeonJeong Lee, Chul-Hyun Cho, Yujin Lee, Jaegwon Jeong. Funding acquisition: Heon-Jeong Lee. Investigation: Heon-Jeong Lee, Chul-Hyun Cho, Yujin Lee, Jaegwon Jeong. Methodology: HeonJeong Lee, Jaegwon Jeong. Project administration: Heon-Jeong Lee. Resources: Heon-Jeong Lee. Supervision: Heon-Jeong Lee, Chul-Hyun Cho, Yujin Lee. Software: Heon-Jeong Lee. Validation: Heon-Jeong Lee, Chul-Hyun Cho, Yujin Lee, Jaegwon Jeong. Visualization: Jaegwon Jeong. Writing—original draft: Jaegwon Jeong. Writing—review & editing: Heon-Jeong Lee, Chul-Hyun Cho, Yujin Lee, Jaegwon Jeong.
